Every two minutes, a woman dies during pregnancy or childbirth. Each day, 6,400 babies die during their first month of life. Most of these deaths occur in low- and middle-income countries. Most are preventable with access to quality health services.
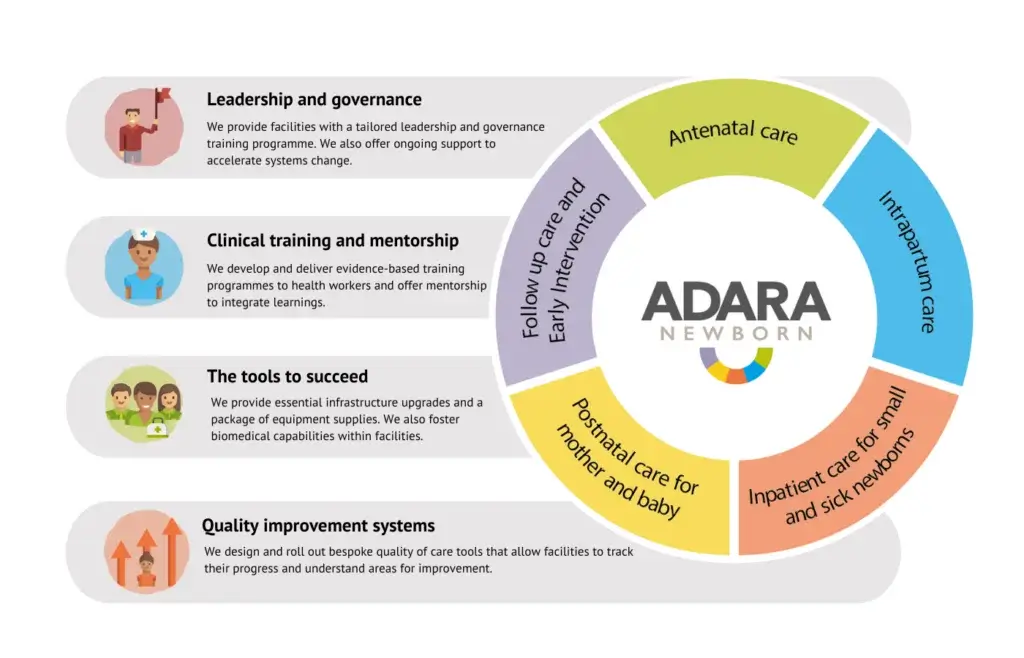
We believe our AdaraNewborn model has the power to halve maternal and newborn deaths and stillbirths across 10 health facilities in Uganda. But saving lives at scale requires a targeted approach to health system strengthening. That’s why AdaraNewborn spans the continuum of care, supporting mothers and newborns from pregnancy through to their return home after birth.
It’s also underpinned by four pillars that strengthen the health system and save lives. Through these pillars, AdaraNewborn provides health workers with training and mentorship; strengthens leadership and governance in the health system; equips facilities with the tools to succeed; and focuses on quality improvement systems. This creates sustainable systems change, saving lives now and reducing maternal and newborn deaths into the future.
Recently, the last pillar – quality improvement systems – has come into sharp focus for our team. As a result, we’ve developed and rolled out bespoke quality of care tools at AdaraNewborn facilities. These allow facilities to track their progress and understand areas for improvement.
Healthcare quality improvement systems
While great strides have been made in improving maternal and newborn health outcomes over the past two decades, progress has begun to stagnate. Uganda is not on track to meet the Sustainable Development Goals (SDGs) for maternal and newborn health. A Lancet report estimates that by 2030 Uganda will still have 21.9 neonatal deaths per 1,000 live births, not meeting the SDG target of 12. To achieve the SDGs, Uganda needs to prevent the deaths of 80,000 newborns over the next decade.
“To bring our AdaraNewborn vision to life, we can’t only focus on increasing accessto health services, we must also improve the qualityof these services,” says Beatrice Niyonshaba, our Uganda Research, Monitoring and Evaluation Manager.
High health care coverage alone is not enough to reduce deaths to reach the SDGs. Increased coverage must be accompanied by improved quality across the continuum of care.
According to the World Health Organization (WHO), quality of care is “the extent to which health care services provided to individuals and patient populations improve desired health outcomes. In order to achieve this, health care must be safe, effective, timely, efficient, equitable and people-centred.” For us, it’s all about delivering the right care to the right people in the right place via the right people with the right skills and resources.
And that’s exactly what AdaraNewborn is working to achieve. By rolling out Healthcare quality improvement tools – hand in hand with training and mentorship, leadership and governance strengthening, and providing facilities with the tools to succeed – we are improving care and saving lives.
“AdaraNewborn is based on our experience working with Kiwoko Hospital which is now recognised by Uganda’s Ministry of Health as a Centre of Excellence in newborn care,” says Beatrice. “And one thing we learnt from working with Kiwoko is that focusing on quality of care – across a broad range of areas – is so important.”
Our recent development and roll out of a quality of care tool showcases the power of this approach.
“Adara’s quality of care tool is based on WHO quality standards and indicators,” says Beatrice. “It monitors the care that is provided and patient experiences of care. It also includes a scoring system to assess compliance to indicators.”
This tool measures quality across a range of areas including routine care, information and referral systems, communication, staffing, training and skillset of the workforce, and infrastructure. This allows facilities to understand the factors that influence quality care, which areas are performing well and where additional opportunities exist.
Quality of care tool in action
We have begun rolling this tool out to our three existing AdaraNewborn sites: Kiwoko, Nakaseke and Luwero hospitals.
“Luwero was the first facility we rolled this tool out to and it was received so well,” Beatrice says. “It’s a truly collaborative process. We hosted workshops to receive input from different stakeholders and across different departments. Everyone was excited to understand how they’re progressing and where there are opportunities for strengthening.”
Based on the results of the tool, we support facilities to develop an action plan for relevant departments. These plans are bespoke and can be tracked quarterly to ensure appropriate steps are being taken to address gaps identified by the tool. These actions are intended to boost quality of care. Facilities are responsible for implementing the plan, guided by a healthcare Quality Improvement Committee
“We want each facility to feel like they own this process,” Beatrice explains. “They’re accountable for driving progress. Adara is here to support them every step of the way. But to create true sustainability in the health system, each facility needs to be the drivers of this journey.”

Following this initial roll out, we will conduct a quality of care assessment each year to measure progress.
“The results we’re seeing now are our baseline,” Beatrice says. “We can see the strengths of each AdaraNewborn facility while also identifying opportunities for growth. We can see where we need to do further training, where the facilities need to carry our infrastructure updates, where we need to work with the district to drive systems change. Over the years, we expect to see quality of care in each facility improve.”
This also allows us to identify emerging issues and develop mitigation strategies. For example, if we find that healthcare staff have not received the appropriate training in essential newborn care and breastfeeding support, then the Healthcare Quality Improvement Committee will work with the hospital management to prioritise strengthening the skillset of the workforce.
And at the end of the day, this will directly translate into lives saved.
future plans
As we enter additional AdaraNewborn facilities, we will roll out our quality of care tool.
To accelerate health care quality improvement globally, we also plan to share this tool with other organisations through the Adara Knowledge Centre, partnerships and conferences.
“While this quality of care tool is just one part of the AdaraNewborn picture, we believe it’s a powerful one,” Beatrice says. “We hope it will contribute to lives saved and changed, across Uganda and beyond.”
Over the next 10 years, we aim to halve newborn deaths and stillbirths across 10 health facilities. We will save 7,000 lives and reach 500,000 women and newborns.
Already, AdaraNewborn is showing excellent results. In 2023 we saw:
- 1,361 babies cared for in the Kiwoko Hospital neonatal intensive care unit (NICU)
- 85% survival rate for newborns in the Kiwoko NICU – an increase from 77% in 2005
- 384 newborns cared for in the Nakaseke Hospital special care baby unit with a 98% survival rate
- 5,777 women cared for across Kiwoko and Nakaseke maternity wards, both with a 99.9% maternal survival rate
That’s a result of increased access to care and improved quality of care for mothers and newborns.

