Imagine giving birth to a premature baby. They’re born small and sick and require inpatient newborn care. You’re a first-time parent, unsure about looking after a baby, let alone one that needs additional support. You live in rural Uganda and when it’s time to take your baby home, you’re nervous.
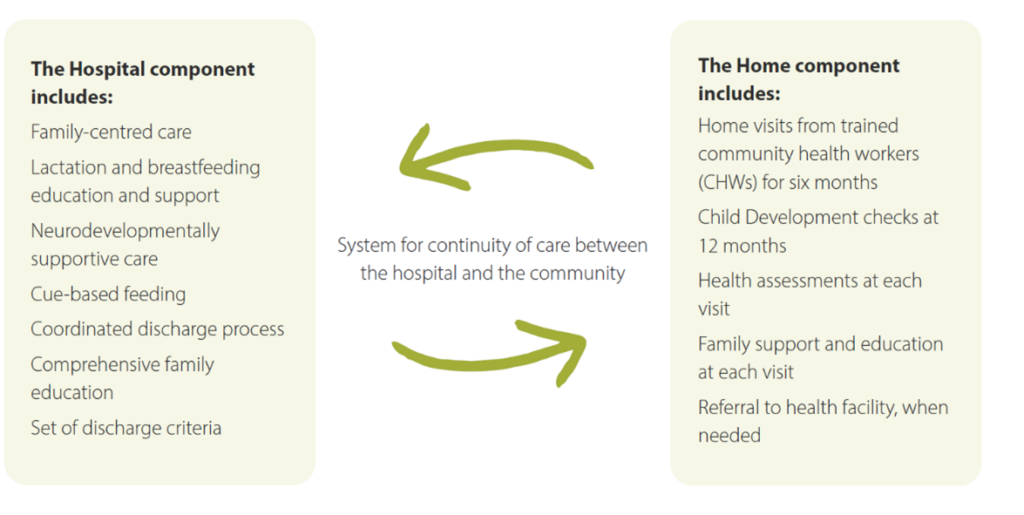
Now imagine having access to a programme that supports you and your newborn both before and after their discharge from hospital. It provides you with comprehensive education during your infant’s stay. It strengthens hospital discharge processes, lactation and breastfeeding practices, and promotes care that encourages healthy brain development.
Then, after discharge, it offers regular at-home follow-up support for six months through a network of volunteer community health workers. The programme builds your confidence and supports your little one, so they grow and flourish.
Over the past 25 years, our work has been informed by a deeply held belief that every newborn has the right to not only to survive but also to thrive. This is why, in 2019, we launched our flagship newborn follow-up programme, Hospital to Home (H2H).
We implemented H2H – the programme described above – across three districts in Uganda. We have believed so deeply in the power of this programme, that we have dreamt of expanding it to other locations to support more families.
This dream led us to develop a “Hospital to Home package” that will allow other organisations to roll out H2H in their facilities and communities. Though H2H is part of our AdaraNewborn model and will be rolled out to all AdaraNewborn facilities, we are proud that it is now also available as a standalone package.
“We look forward to seeing this programme implemented in other sites, supporting countless newborns to flourish,” said Daniel Kabugo, our Uganda Country Director. “The data has shown us the power of Hospital to Home. As an organisation committed to sharing our knowledge, we believe it is now important that we share this work with others.”
This package is targeted at health professionals or leaders working in hospitals in low-resource settings who want to decrease the risk of preventable newborn deaths. It includes all the materials and instructions necessary for other facilities to implement their own H2H programme. This consists of guidelines covering breastfeeding and neuro-developmentally supportive care, training packages, job descriptions and reporting templates.
“Both components of the H2H programme are important and complement each other,” Daniel explains. “The hospital component is the foundation for caregivers to learn how to care for their high-risk newborns. The home component ensures infants and their families receive ongoing nurturing care during a critical period of their development.”
In developing this package, we have also understood that challenges such as financial or resource constraints may limit an organisation’s ability to implement the whole programme at one time. A single component may be implemented to start, depending on hospital readiness and existing services, with additional components added over time.
We have heard that there is a crucial need for a follow-up programme like H2H from many people across Uganda and the world. We believe it is the first of its kind. The package has been endorsed by the Uganda Ministry of Health who expressed the shared goal of wanting to see this programme scaled to other public facilities across the country. We are already in conversations with organisations who wish to begin rolling it out.
Cornety Nakiganda, a midwife of more than 40 years, has been leading the “hospital” component of the programme since it launched in Central Uganda in 2019. She is thrilled to see this expansion of the programme.
“It is our hope that this programme will be rolled out across Uganda and the world,” Cornety says. “We want to see stories of success recreated not only for families in Central Uganda, but in places like Rwanda, Ethiopia and even Nepal.”


