Babies born sick and small have an increased risk of complications. As a result, many need intensive medical care. The neonatal intensive care unit (NICU) is a hospital ward with specialist medical staff and equipment to care for premature and sick newborns.
While some babies may only need short-term observation, others face complex health challenges that require intensive treatments.
Each year, hundreds of thousands of small and sick newborns in low- and middle-income countries die because medical facilities do not have the equipment to help babies survive in those crucial first few weeks of life. Many of these deaths are preventable.

AdaraNewborn
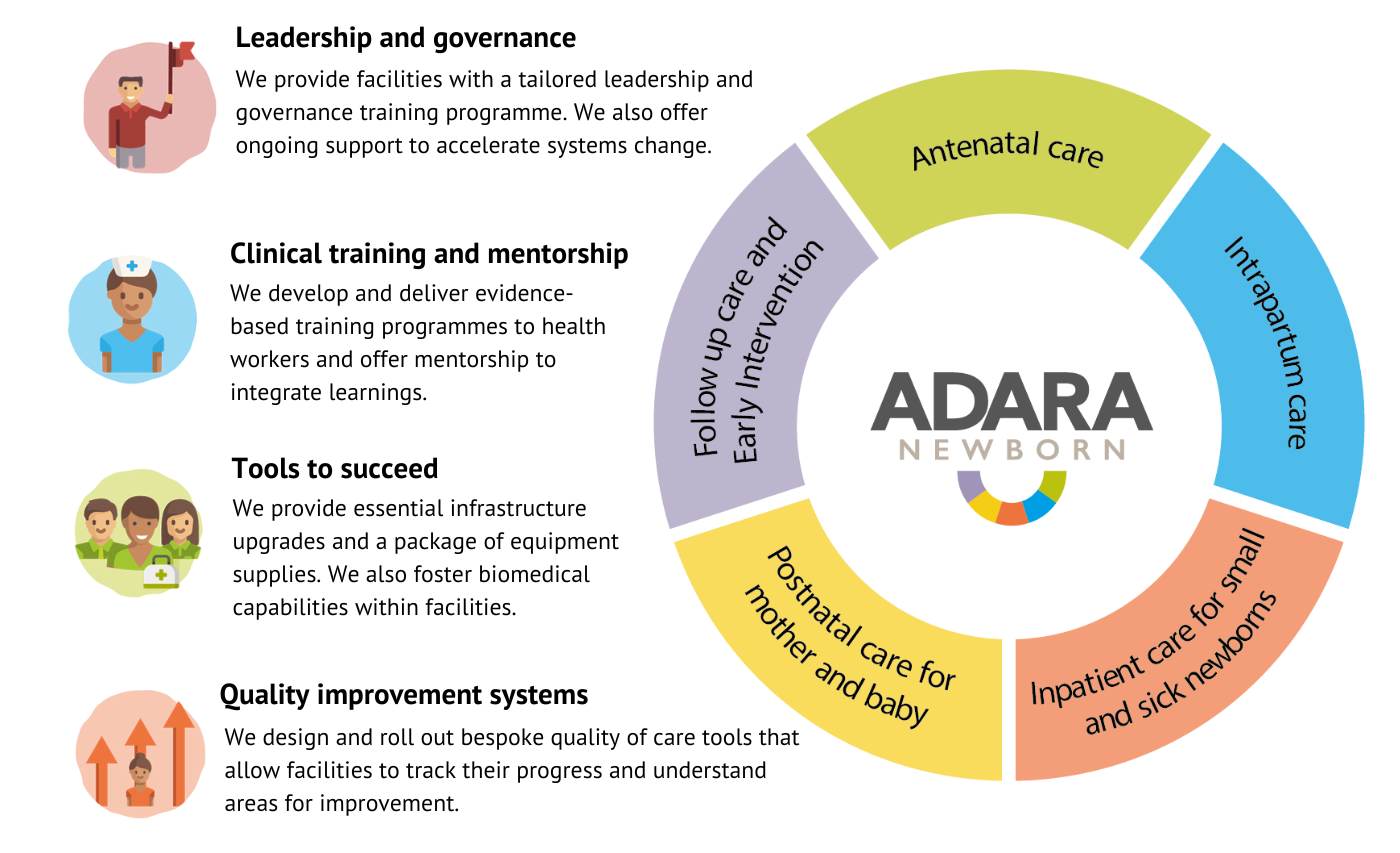
We’ve pioneered a model – AdaraNewborn – for increasing survival rates for the sickest and smallest newborns and their mothers to meet Sustainable Development Goal (SDG) targets. Our model ensures facilities and newborn units are resourced with the equipment, staff, training and infrastructure needed to save lives. We have already begun expanding this work and we currently operate AdaraNewborn in three sites across Uganda, where newborn disorders are the leading cause of death.
AdaraNewborn spans the continuum of care, supporting mothers and newborns from pregnancy through to their return home after birth. Caring for babies in the newborn intensive care unit falls into the third arm of the model – ‘inpatient care for small and sick newborns.’ Through this, we provide training focused on quality care, rooted in the fundamentals of newborn care. By prioritising specialised care and support for premature infants, we aim to bridge the gap in survival rates and ensure that every newborn has the chance to thrive.
Kiwoko Hospital is at the centre of this work as our first AdaraNewborn site. From 24 years working with Kiwoko, we have developed a depth of knowledge in the care of newborns. As a result, it is now a leading NICU in Uganda and is recognised as a Centre of Excellence in newborn care by the Ugandan Ministry of Health. In 2023, 1,352 newborns received care in the Kiwoko NICU, with an 85% survival rate – up from 77% in 2005. As we strive to halve maternal and newborn deaths and stillbirths through AdaraNewborn, we are establishing high-quality newborn units at 10 facilities.
As we scale AdaraNewborn model across the country, Kiwoko will sit at the heart of our first regional hub as a referral facility that can provide higher levels of care while also modelling what is possible in newborn health.
NICUs, like Kiwoko, play a critical role in reducing neonatal mortality rates by providing babies with the specialised care they need to survive and thrive. Premature birth, respiratory distress syndrome, and birth asphyxia are among the most common conditions treated. You can read more below about these conditions and how AdaraNewborn is saving newborn lives.
Prematurity
Prematurity is one of the most common reasons newborns are admitted to the neonatal intensive care unit. Babies born before 37 weeks of pregnancy are considered preterm.
Premature infants often face a range of complications due to their underdeveloped organs, particularly their lungs, brain, and digestive systems. These babies may have difficulties maintaining their body temperature, feeding, and breathing on their own. The NICU offers specialised treatments and care for these babies, ensuring that they receive the attention and care needed to grow strong and healthy.

While prematurity is common, there are stark inequalities in survival rates across the globe with many lives needlessly lost. In fact, prematurity is the leading cause of death in children under five years worldwide. Many of these deaths occur in low-income countries. In these places, half of all babies born very premature (at or below 32 weeks) lose their lives due to a lack of accessible, cost-effective care. In high-income countries, almost all these babies survive.
At Adara, we’re privileged to work with newborns, including those born too soon. We’re also fortunate to work with the dedicated staff providing life-saving care to these babies. Preventing deaths and complications from preterm birth starts at pregnancy. That’s why AdaraNewborn works to address the quality and availability of services across the continuum of newborn care, supporting mothers and newborns from pregnancy through to their return home after birth.
Respiratory distress syndrome
Respiratory distress syndrome (RDS) is a common and serious condition in premature infants. It occurs when a baby’s lungs are underdeveloped, making it difficult for them to breathe properly.
RSD is the most frequent cause of disease and death for babies born before 34 weeks. In low- and middle-income countries, newborns face a significantly higher risk of complications or death from RDS. Many health facilities lack the essential equipment and resources needed to treat this condition, leading to preventable neonatal mortality.
For many years, we have worked with PATH , Seattle Children’s University of Washington and Kiwoko Hospital to develop an innovative a bubble continuous positive airway pressure (bCPAP) device. This device can help manage newborns with respiratory distress and supports babies to breathe and survive.
In 2021, together with our partners, we conducted a trial of this device in the Kiwoko Hospital neonatal intensive care unit. The device was found to be feasible in a Ugandan level two newborn unit and acceptable to healthcare workers experienced in bCPAP and oxygen blending. The effective use of such devices in referral and district hospitals could prevent 178,000 newborn deaths in Africa each year. We believe countless lives could be saved by making this technology available across low- and middle-income countries worldwide.

Birth asphyxia
Another common condition treated in the neonatal intensive care unit is birth asphyxia, which occurs when a baby doesn’t get enough oxygen before, during, or just after birth. This lack of oxygen can lead to serious complications, including brain damage, organ failure, and even death if not treated quickly.
Proper medical care, treatment and monitoring before and after birth can help reduce the impact of birth asphyxia. It remains a leading cause of neonatal mortality and morbidity in low- and middle-income countries. Most deaths could have been prevented with timely intervention and treatment.
n late 2023, we published birth asphyxia research from Kiwoko Hospital in PLOS Global Public Health. It found that increasing capacity in lower-level facilities for birth and newborn care may reduce the incidence of birth asphyxia, improve outcomes and help meet newborn mortality targets.
The study observed that the risk of death due to birth asphyxia was twice as high when babies arrived from another facility as when they were born at Kiwoko Hospital.
AdaraNewborn strives to uplift quality of care in health facilities to save lives. It emphasises the importance of antenatal care to identify problems early; lifts quality of intrapartum care; trains and mentors health workers; provides facilities with the tools they need to succeed; and strengthens referral networks through a hub and spoke model. According to this new research, these factors may reduce the incidence of birth asphyxia. This showcases the power of AdaraNewborn to reduce newborn mortality.

The neonatal intensive care unit plays a vital role in providing life-saving care to small and sick newborns, ensuring they receive the specialised care they need. Unfortunately, too many newborns are dying of preventable conditions in low- and middle-income countries. AdaraNewborn has power to halve newborn deaths and stillbirths across 10 health facilities in Uganda over the next decade. Through this work, we will reach half a million women and save over 7,000 lives. By demonstrating the impact of AdaraNewborn in Uganda, we will support other countries to adapt and adopt the model. Join us as to ensure every newborn has access to the care they need to survive and thrive.

